How does your team measure and optimize on on-boarding costs? If you are not sure how to answer this question, we will show you how to evaluate and ways you can minimize your on-boarding burn on your team.
Methodology
First let’s do a quick review of our methodology. The key metric used for evaluating on-boarding performance is on-boarding costs per shift.
On-boarding Cost / Shift
Where
On-boarding Costs = Vetting Costs + Credentialing/Enrollment costs + Training and On-boarding Costs
In our view on-boarding includes all vetting, credentialing, training and training resources required to bring a new provider on board across all hired and un-hired physicians. What do we mean by hired and unhired? We want to make sure we are evaluating the time spent vetting candidates that are not a match or that do not make it through credentialing. This is an example of waste, where the time spent reviewing presentations, interviewing candidates, or credentialing results in no covered shifts. We will get into specific examples of how to minimize your acquisition costs by specific variable.
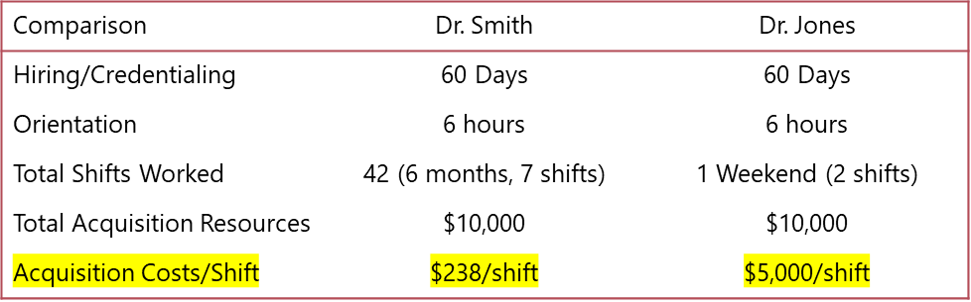
The other important component of this measurement is how you can increase your shifts per provider acquired, or rather your retention. Because acquisition costs are fixed, the fewer providers you have to train/vet/credential, the lower the team administrative burden. Let’s look at a quick example on leveraging acquisition costs:
How to minimize On-boarding Costs?
Hiring/Vetting
measure with % of presentations accepted
In order to make sure you have well matched candidates you must have a thorough description of the credentials required, procedures and skills or responsibilities. If you outline exactly what you require as well as the practice setting, candidates will also know more about the opportunity. Because it takes time to review a presentation file and schedule and interview candidates, minimizing the number of candidates reviewed per hire is crucial. Another very important aspect of hiring when working with multiple agencies is standardizing the presentation format so every consistent. This will ensure quicker review and easier comparison across candidates. Don’t have a template? We can help you with that.
Larger health systems and provider groups should also share information on locum recommendations on providers to facilitate the vetting process.
Credentialing
measure with Average Credentialing Days
Delayed credentialing can be very burdensome and stressful on a team, especially a team that needs providers urgently. Here are a couple items to make sure credentialing goes smoothly:
· Ensuring that all your agencies know the checklist of your specific Medical Staff Office and meeting schedule. Some MSOs require specific references and the more time agencies know this in advance, the faster they can get materials together.
· Setting up shared updates can make sure everyone is on the same page including the provider.
· Utilizing prioritization guidelines to make sure the most urgently needed candidates are getting through first.
· You should give your MSO office notice if there will be a high volume of candidates coming through to make sure they are prepared.
Training/On-boarding
Here are some suggestions to ensure smooth and efficient on-boarding:
· Implement a thorough and standard on-boarding checklist (We made one for you here).
· Leverage group orientation sessions or any online training materials
· Utilize administrative staff and nurse managers to help on tours to alleviate burden on medical director’s times
How to maximize Shifts/acquired Physician?
Retention (measure with average shifts per provider)
A large part of retention is making sure the providers are set up for success and have been fully trained and on-boarded. Best practice is to also check in and ensure the provider is comfortable with the systems, workload and acuity level. The highest cause of locum turnover is due to expectations not in line with reality (learn more in our 5 Most costly Locum Mistakes article). Closing the feedback loop on locum satisfaction is important for retaining interim physicians.
Culture (survey)
Are the physicians, nursing staff and rest of the facility (consultants etc.) aware that your practice is staffing locums? Most believe that compensation is the only way to draw physicians to your practice but there is also a quality of life component which can be utilized as a selling point. Practice reputation can have both favorable and unfavorable impact on both recruiting and retaining locums as well as full time recruits.

